A recent Harvard University and Massachusetts Institute of Technology (MIT) scientific stem cell study is a breakthrough for people with diabetes. Scientists of this important advancement in the field of stem cell research used embryonic stem cells to create billions of pancreatic beta cells capable of producing insulin.
Patients with type 1 diabetes as well as some patients with type 2 diabetes may find this scientific breakthrough very encouraging. Additionally, those patients needing daily injections of insulin because their body is incapable of producing the hormone on its own may find this advanced study a ray of hope and substantial benefit.
Douglas A. Melton, Ph.D. is the Xander University Professor at Harvard University and an Investigator of the Howard Hughes Medical Institute. In addition, he is also a co-director of Harvard’s Stem Cell Institute and Co-Chair of the Department of Stem Cell and Regenerative Biology at Harvard University. Dr. Melton explains, “We are now just one preclinical step away from the finish line.”
The “one preclinical step” Dr. Melton is referring to is finding a safe way to stop the immune system from destroying the newly formed cells.
Stem Cell Research and Diabetes
Advanced levels of blood sugar in the human body can damage organs and tissues. Insulin is a hormone made by the pancreas. Insulin allows the body to use sugar, or glucose from carbohydrates in the food consumed for energy or to store glucose for use in the future. Insulin also helps keep the body’s blood sugar level from getting too high or too low.
Type 1 diabetes is an autoimmune disease in which the body destroys insulin-producing beta cells in the pancreas. The human body cannot control glucose without insulin.
The researchers of this ground-breaking study explain that in order for the new technique to work in people with type 1 diabetes, the researchers need to add another component that is capable of stopping a recipient’s immune system from attacking close to 150 million beta cells they would receive.
The team of researchers collaborated with other professionals at the Massachusetts Institute of Technology (MIT) in an attempt to develop an implant that protects stem cell derived beta cells from being attacked by the immune system of patients.
According to Dr. Melton, a device is currently being tested. So far, the device created by the scientists is working. Beta cells implanted in mice months ago are still protected. Dr. Melton says, “They are still producing insulin.”
One of the Most Important Advances in the Field of Stem Cell Research
Howard Hughes Medical Institute investigator, Elaine Fuchs, Ph.D. of Rockefeller University is not involved in the study.
However, Dr. Fuchs says, “I join the many people throughout the world in applauding my colleague for this remarkable achievement. For decades, researchers have tried to generate human pancreatic beta cells that could be cultured and passaged long term under conditions where they produce insulin. Melton and his colleagues have now overcome this hurdle and opened the door for drug discovery and transplantation therapy in diabetes.”
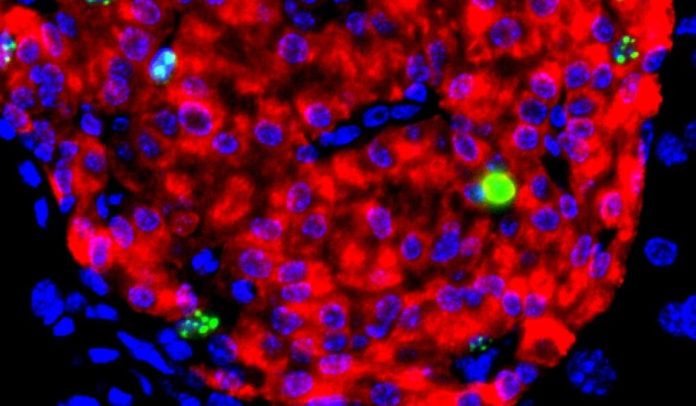
Dr. Melton and his colleagues say their stem cell differentiation method can create hundreds of millions of glucose-responsive beta cells that have all the characteristics of mature beta cells.
They can secrete quantities of insulin comparable to adult beta cells in response to various glucose challenges, package insulin into secretory granules, produce a calcium ion response to glucose, and express markers found in mature beta cells.
“Furthermore,” they clarify, “these cells secrete human insulin into the serum of mice shortly after transplantation in a glucose-regulated manner, and transplantation of these cells ameliorates hyperglycemia in diabetic mice.”