Intimate partner violence (IPV) is the leading cause of non-fatal injury to women worldwide. Musculoskeletal injuries, which are often seen by orthopaedic surgeons, are the second most common manifestation of IPV. We aimed to establish the 12-month and lifetime prevalence of IPV in women presenting to orthopedic fracture clinics.
The PRAISE team of 80 investigators did a cross-sectional study of a consecutive sample of 2945 female participants at 12 orthopedic fracture clinics in Canada, the USA, the Netherlands, Denmark, and India. Participants who met the eligibility criteria anonymously answered direct questions about physical, emotional, and sexual IPV, and completed two previously developed questionnaires (Women Abuse Screening Tool [WAST] and Partner Violence Screen [PVS]), response rate 2,334 women. Researchers did a multivariable logistic regression analysis to investigate the risk factors associated with IPV.
Sheila Sprague, MSc. Department of Clinical Epidemiology and Biostatistics at McMaster University in Ontario, and colleagues, investigated the occurrence of intimate partner violence seen in the orthopedic surgical setting and found among the respondents that one in six women (16%) disclosed a history of IPV within the past year, and one in three (34.6%) had experienced IPV in their lifetime.
In addition 49 women (1.7%) attended their clinic visit as a direct consequence of IPV, and only seven of them (14%) had ever been asked about IPV in a health-care setting.
Sprague said the surprisingly high rate high rate of domestic violence suggests that fracture clinics are good locations to target screening and intervention programs aimed at victims of domestic abuse.
“Intimate partner violence is far more prevalent among female patients presenting at fracture clinics than has been generally recognized.” “Surgeons need to be aware of this and they need to feel comfortable asking their patients about it.” related Sprague to MedPage Today.
Women in short-term relationships (OR 0·584, 99% CI 0·396—0·860, p=0·0001) were at increased risk of IPV and physical abuse in the past 12 months in this study.
The study also found that among the women surveyed 16% experienced emotional abuse, 18% physical abuse and just fewer than 10% had experienced sexual abuse at some point in the past.
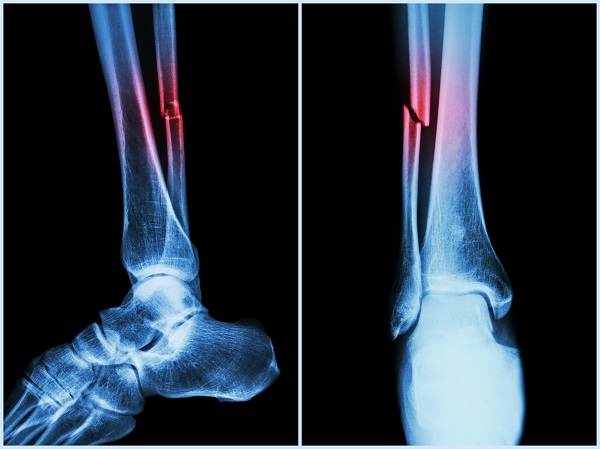
The most common injuries related to intimate partner violence were; 18% fractures of the foot or ankle 14% hand or wrist fractures and other fractures in more than one location 18%.
Being in a relationship of less than a decade in duration, being unmarried, and having children were common characteristics of women at risk for intimate partner violence.
Among the women in the survey about three-quarters had said they believe healthcare providers should ask their female patients about domestic violence, and about two-thirds agreed that orthopedic surgeons should discuss the issue with their patients.
The U.S. Preventive Services Task Force (USPSTF) recommends that clinicians screen women of childbearing age for intimate partner violence and provide or refer women who screen positive to intervention services (B recommendation).
In a past study, Sprague and colleagues completed a cross-sectional study of 282 injured women attending two Level-I trauma centers in Canada. The team found generally underestimated the rate of domestic violence among their patients.
In this study “Most had suspected domestic abuse, especially in cases where a patient’s story didn’t align with her injuries.” “But they didn’t know what to do. We need to educate orthopedic surgeons so that they know what to look for and help them develop a plan of action.” said Sprague.
She adds at the very least fracture clinics should be able to refer women who are victims of domestic violence for help. Ideally, fracture clinics could have formal intimate partner violence screening programs in place administered by a social worker or a nurse.
In their interpretation the team writes “Our findings warrant serious consideration for fracture clinics to improve identification of, respond to, and provide referral services for, victims of IPV.”
In a commentary to the study, Professor Kelsey Hegarty, MBBS, FRACGP, DipRACOG, PhD, Associate Professor and leads the Abuse and Violence research program in the Primary Care Research Unit, Department of General Practice, University of Melbourne had wrote “Not all clinicians and staff are able to ask about domestic violence, or they might not be suited to doing so.” “The onus should be on hospital and clinic systems to enable and support clinicians who suspect domestic violence to suggest to women a referral service that could assist them with any emotional issues associated with their presentation” as reported by MedPage Today.
She added that while many patients may not be ready to name their problem as domestic violence, they might be open to accepting help for emotional issues.
This study appears in the June 12th issue of The Lancet.
In 2010, violent crimes by intimate partners (both male and female) totaled 509,230 and accounted for 13 percent of violent crimes.
According to Women’s Health.org Domestic violence is when one person in a relationship purposely hurts another person physically or emotionally. Domestic violence is also called intimate partner violence because it often is caused by a husband, ex-husband, boyfriend, or ex-boyfriend. Women also can be abusers.
People of all races, education levels, and ages experience domestic abuse. In the United States, more than 5 million women are abused by an intimate partner each year.